Christopher Ravn
Key Takeaways
1. Sundowning typically becomes more prominent as dementia progresses, particularly in the mid to late stages, such as with Alzheimer’s disease. Symptoms may intensify with deeper cognitive decline, leading to increased restlessness, agitation, and hallucinations in the later stages.
2. Sundowning can manifest at various points in Alzheimer’s disease, becoming more noticeable as cognitive decline deepens. While early-stage occurrences may be less pronounced, symptoms tend to become more obvious with disease advancement, highlighting the importance of recognizing typical progression patterns.
3. Sundowning in dementia patients can be triggered by various factors, including fatigue, changes in lighting, disruptions in routine, and seasonal variations. Understanding these triggers is essential for caregivers to implement strategies that create calm, supportive environments and effectively manage symptoms.
Table of Contents
1. What Stage Of Dementia Is Sundowning?
2. At What Point Does Sundowning Begin In Alzheimer’s?
3. Why Does Sundowner's Occur In People With Dementia?
4. What Exactly Triggers Sundowning In Dementia?
5. How Long Can Sundowning Episodes Last?
6. Sundowner’s Symptoms And Behavioral Changes In Dementia
7. Does The Change Of Seasons Influence Sundowning?
8. How To Manage Sundowning
9. Can Sundowning Be Treated?
10. Understanding Sundowning In Dementia And Alzheimer’s
11. Frequently Asked Questions About What Stage Of Dementia Is Sundowning
What Stage Of Dementia Is Sundowning?
Though common, sundowning is a rather challenging phenomenon in dementia, particularly with Alzheimer’s disease that presents itself during the mid to late stages of the disease. This phenomenon can occur at any stage but is more prominent with the progression of dementia.
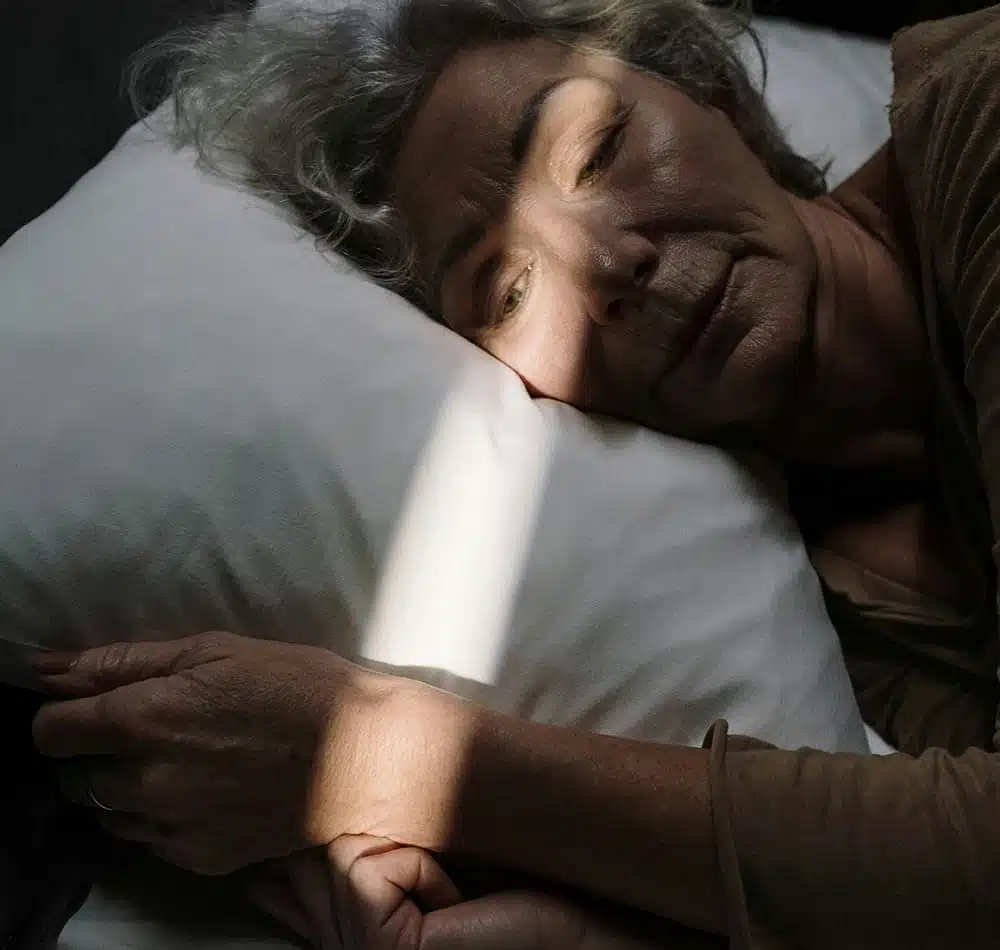
Here we explore the ties between sundowning and the various stages of dementia and how it presents with the progression of the disease. During the early stages of dementia, mild instances of agitation and confusion occur late in the afternoon or evening. Yet with the progression of dementia, symptoms of sundowning tend to intensify, with patients becoming more restless, agitated, and may even hallucinate in later hours of the evening.
For caregivers to anticipate and manage the problems they experience with sundowning, they need to understand it. By observing the typical advancements of sundowning through the stages of dementia, caregivers can carry out strategies to reduce symptoms and adequately support the patient experiencing this problem.
At What Point Does Sundowning Begin In Alzheimer’s?
The onset of sundowning in Alzheimer’s Disease is highly challenging and differs between individuals at various stages of the disease. In general, sundowning tends to manifest in the mid to later stages of Alzheimer’s, though some have experienced it in early stages. Also, in early-stage occurrences, the sundowning symptoms may not be as noticeable. It becomes more pronounced with deepening cognitive decline as the disease advances and the behaviors become more obvious.
In the early stages of Alzheimer’s, individuals may not exhibit noticeable sundowning symptoms. However, as the disease progresses and cognitive decline deepens, sundowning behaviors may become more apparent. Typically, sundowning manifests as increased confusion, agitation, restlessness, or mood swings during the late afternoon or evening hours.
To comprehend the likely onset of sundowning in Alzheimer’s is imperative for caregivers to plan and manage the symptoms effectively. Recognition of typical progression patterns in the disease and awareness of sundowning signs give caregivers the ability to carry out strategies in minimizing triggers and better support their patient to navigate these times.
Why Does Sundowner's Occur In People With Dementia?
A common phenomenon in dementia called sundowning occurs with the combination of factors involving both changes in the brain and triggers in the environment.
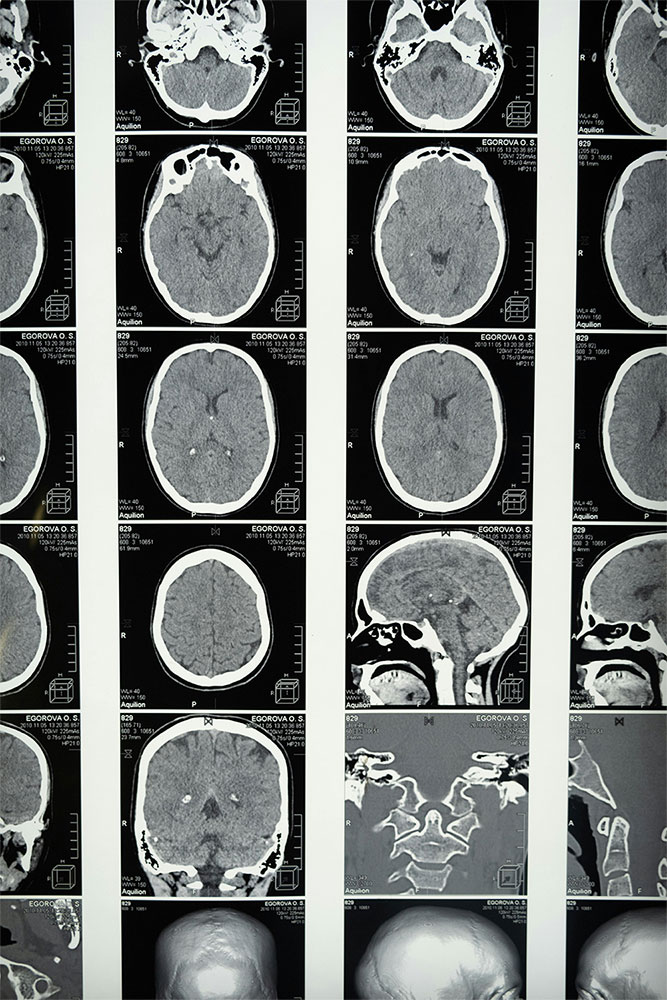
The internal clock, or circadian rhythm regulating sleep-wake cycles, disregulation has been cited as a potential cause of sundowning in dementia patients. The rhythm disregulation leads to increased agitation and confusion most prominently in the late afternoon or evening – hence the terminology “sundowning”.
Furthermore, brain changes related to dementia, for example, damages in areas that regulate emotions and behaviors, can bring about episodes of sundowning. Environmental factors, such as poor lighting or increased noise levels later in the day, can agitate symptoms. Thus, it is important to get gifts for dementia patients that help them with this situation.
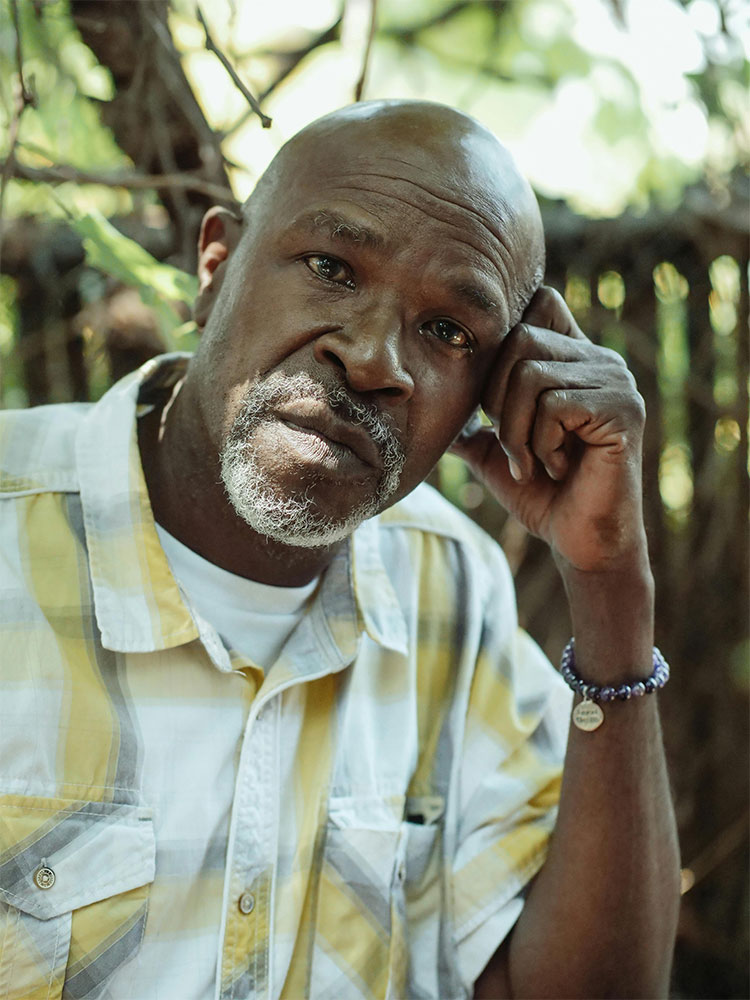
Caregivers need to understand the multifaceted characteristics of sundowning to impose strategies that soothe the effects. Both biological and environmental factors have to be managed for caregivers to create a comprehensive support system that calms the surroundings for dementia patients in the midst of sundowning.
What Exactly Triggers Sundowning In Dementia?
Various factors can trigger sundowning in dementia, each impacting the onset and precipitation of symptoms.
Fatigue and exhaustion are common triggers, making dementia patients more vulnerable to agitation and confusion as they become tired. Lighting changes and shadows, especially with artificial light being used more, can trigger sundowning episodes. Visual disturbances are heightened by the contrast between light and shadow, creating even greater disorientation.
Additionally, changes in the environment and personal routine, such as the natural transition from an active day to a peaceful night, can disrupt dementia patients, making them vulnerable to sundowning. By examining triggers, caregivers can better understand and be prepared to recognize the onset of sundowning symptoms and already be equipped with the knowledge of proactive measures to reduce their impact and give adequate support to the patients with dementia in their turmoil.
Early Signs Of Sundowning In Dementia Patients
Seeing and taking prompt action when the early signs of sundowning show up is crucial for a prompt and appropriate response. Early signs involve restlessness, irritability, or greater confusion in the late afternoon to early hours of the evening. Subtle shifts in the behavior of dementia patients indicate the early onset of sundowning before escalation. Thus, it is also important to find ways on how to help someone with dementia remember the time and the day.
Vigilance in responding to early sundowning signs helps mitigate the effects of sundowning by creating a calmer, more supportive environment. These mitigating factors may involve creating an atmosphere of calm with soothing music and low lights. Furthermore, early intervention helps avoid worsening of symptoms and serves to reduce distress for both dementia patients and their caregiver.
How Long Can Sundowning Episodes Last?
The duration of sundowning differs greatly between patients and fluctuates within the individual over time. Generally, sundowning usually lasts a few hours between late afternoon and early evening, though certain episodes persist for longer or shorter time spans relating to factors like the severity of their dementia, environmental triggers, and how well the individual responds to help.
It has also been observed that the rate of progression with sundowning mirrors the advancement of dementia stages. The frequency of sundowning increases with the progression of dementia, signaling the overall decline of brain activity and behavioral functions. Understanding the expected timeline of sundowning and its relationship with the stages of dementia can help caregivers better plan and manage the problems that arise from these manifestations and more effectively maintain a better quality of life for the individual facing dementia.
We Believe Prioritizing Brain Health Enhances Your Quality Of Life
Get to know our team, our mission and how our EVY LIGHT® can provide you and your loved ones with a fuller life, letting you breathe a little easier.
Sundowner’s Symptoms And Behavioral Changes In Dementia
The common symptom of dementia known as sundowning manifests through various behavioral changes, including confusion, agitation, and anxiety, typically occurring from late afternoon to early evening. Sundowning symptoms differ from normal changes in behavior caused by dementia, as they are often more pronounced and only occur during specific times of the day.
It is imperative for caregivers to differentiate between sundowning and other common behaviors of dementia in order to best support the patient. Understanding and compassion are critical in creating a calming environment and implementing strategies to alleviate stress during these episodes. Caregivers should provide empathetic care to enhance the overall well-being and quality of life for those with dementia experiencing sundowning.

Does The Change Of Seasons Influence Sundowning?
Sundowning can also be influenced by seasonal changes for individuals with dementia. Fluctuations in temperatures and variations in daylight can disrupt the body’s internal clock, exacerbating symptoms related to sundowning. The circadian rhythm is disrupted by the changing daylight exposure during seasonal transitions, leading to increased confusion and agitation in the late afternoon and early evening. Additionally, the changing light conditions caused by shorter daylight hours and poorer natural light quality can distort perceptions of time, contributing to the onset of episodes.
It is crucial to recognize the impacts of sundowning for caregivers in order to manage the potential effects. Making adjustments to the environment, maintaining more consistent daily schedules, and providing tailored support for the individual experiencing sundowning are necessary to help mitigate the impact of seasonal transitions on the patient year-round.

Enhance your brain performance through the power of light.
Comfortable and easy to use 40Hz light therapy to support and improve your brain function.
View Our LightHow To Manage Sundowning
The management of sundowning involves a multifaceted approach to address individual needs and environmental factors. Environmental adjustments such as maintaining consistent daily routines, improving lighting conditions, and reducing noise levels help mitigate triggers by creating calm atmospheres. Additionally, caregivers play critical roles in attempting to prevent wandering, a common and potentially dangerous behavior during sundowning, by implementing safety measures such as door alarms or calmly redirecting the individual.
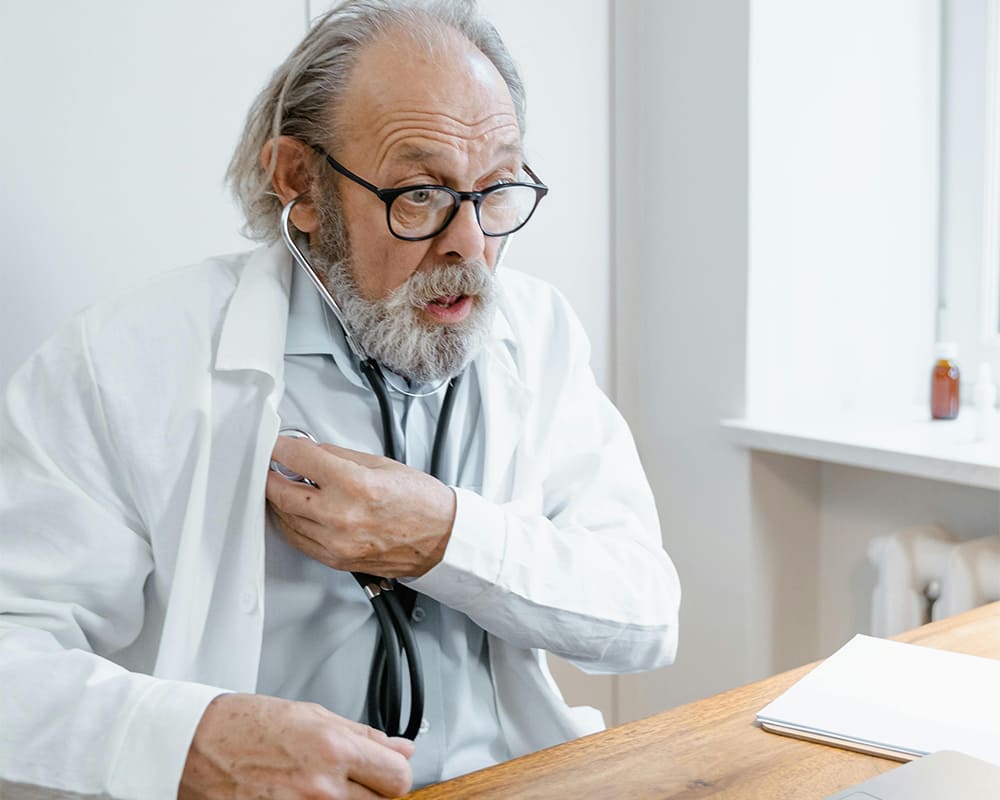
In certain cases, medication may be necessary to help alleviate symptoms, and this should be done under the guidance of healthcare professionals who consider the potential side effects. By understanding how room layout, noise levels, and lighting impact or exacerbate sundowning, caregivers can proactively make environmental changes to support their patient’s comfort and reduce stress.
Can Sundowning Be Treated?
Sundowning can be treated with a combination of medications and non-pharmaceutical interventions. Non-pharmaceutical approaches are often employed first to ensure a conducive environment and routine for the patient, along with behavioral management techniques to address anxiety and agitation. Participating in stimulating activities while limiting caffeine and sugar intake helps regulate the circadian rhythm, thereby reducing sundowning symptoms.
In some cases, non-pharmaceutical interventions may be insufficient. Healthcare professionals may then consider prescription medications such as antidepressants, antipsychotics, or sleep aids, used carefully and closely monitored for potential side effects and negative interactions with other medications. Each treatment for sundowning should be tailored to the individual, focusing on improving overall quality of life and well-being.
Understanding Sundowning In Dementia And Alzheimer’s
Sundowning in Alzheimer’s and dementia patients is characterized by behavioral changes such as agitation, confusion, and anxiety that typically occur during a specific evening period, starting from late afternoon. Seeking perspectives from experts and other caregivers involved in the patient’s care and well-being is imperative to better understand the associated challenges and characteristics.
This understanding is crucial for caregivers to employ effective strategies for mitigating episodes of sundowning while providing compassionate care. However, recognizing the deeper implications of sundowning in dementia and Alzheimer’s patients, as well as their families, highlights the need for more holistic support systems and tailored interventions to improve the quality of life. The comprehensive management of sundowning allows caregivers to create and foster environments of comfort, security, and well-being for those impacted by dementia and Alzheimer’s disease.
Learn What Others Have Experienced with EVY Light
See how others have achieved a sharper mind by activating their gamma brainwaves in combination with maintaining a healthy lifestyle.
Frequently Asked Questions About What Stage Of Dementia Is Sundowning
What Stage Of Dementia Is Sundowning?
Can Sundowning Be Treated?
Sundowning can be treated with a combination of medications and non-pharmaceutical interventions.