Christopher Ravn
Key Takeaways
1.Alzheimer's disease typically progresses over several years through seven stages, with each stage marked by distinct symptoms and challenges indicating advancement to the next stage.
2. The duration of each stage varies between individuals, but generally, the early stages involve mild cognitive decline lasting for years, while the later stages, characterized by severe cognitive decline, can vary from months to several years.
3. As Alzheimer's progresses, extensive care and support are needed, with a focus on maintaining comfort and dignity in the final stages. End-of-life planning becomes essential, with a focus on symptom management and preserving quality of life.
Table of Contents
1. How Long Do The 7 Stages Of Alzheimer's Last?
2. What Are The 7 Stages Of Alzheimer's?
3. What Happens After Stage 7 Alzheimer's?
4. Alzheimer’s Disease Timeline
5. Which Stage Of Alzheimer's Is The Longest?
6. How Long Does Stage 7 Alzheimer's Last?
7. How Long Is Stage 6 Alzheimer's?
8. Stage 5 Alzheimer's Memory
9. Transition Signs Between Seven Stages Of Alzheimer’s
10. Alzheimer's Life Expectancy
11. Frequently Asked Questions About How Long Do The 7 Stages Of Alzheimer's Last
How Long Do The 7 Stages Of Alzheimer's Last?
Understanding the duration and progression of Alzheimer’s disease is crucial for caregivers and families as they navigate its challenges. The progression of Alzheimer’s typically spans several years, with each stage marked by new symptoms and challenges indicating advancement to the next stage.
In the initial stage, individuals may experience mild cognitive decline, which can last for years. Symptoms include subtle memory lapses and difficulty concentrating. As the disease progresses through stages two to six, symptoms intensify, including confusion, disorientation, and a decline in the ability to perform daily tasks independently. In the final stage, characterized by severe cognitive decline and loss of motor function, the duration can vary from months to several years.
It’s important to recognize that the progression of Alzheimer’s varies between individuals due to factors such as age, overall health, and genetics. Some may experience a more rapid decline, while others progress more slowly through the seven stages. Understanding these differences is essential for tailoring care plans and providing optimal support to patients and their families throughout the course of the disease.
What Are The 7 Stages Of Alzheimer's?
Understanding the distinct patterns and challenges of each of the 7 stages of Alzheimer’s is crucial for both patients and their caregivers.
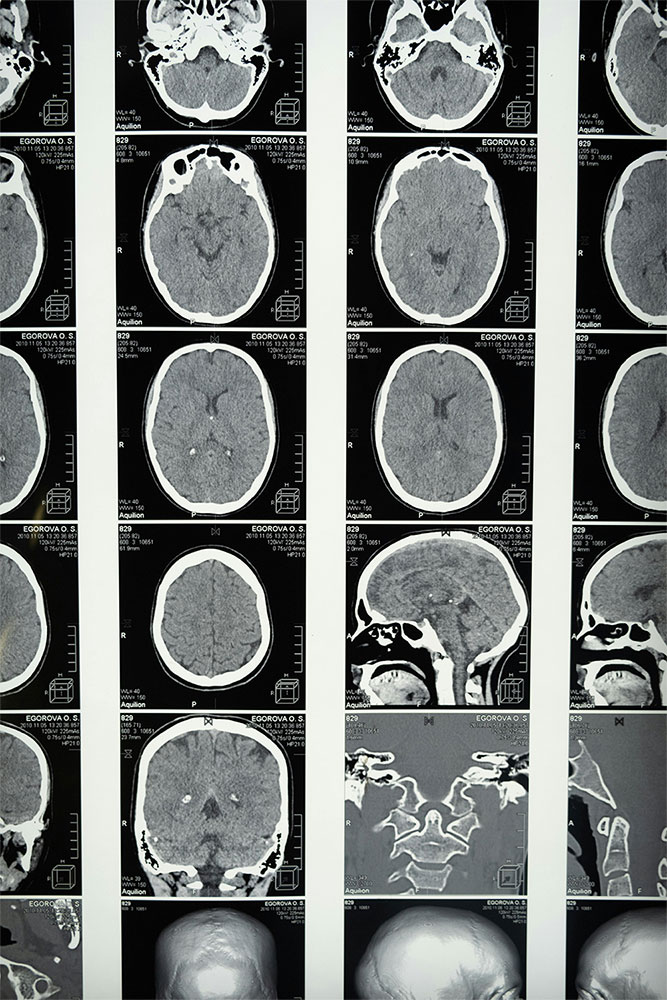
Preclinical Stage: In this stage, there are no discernible symptoms, but changes are occurring in the brain.
- Stage 1: Characterized by mild cognitive decline, including memory lapses and difficulties with concentration. Patients may begin to forget familiar words or names.
- Stage 2: Early Alzheimer’s stage where mild cognitive decline and memory lapses start to impact work and social life. Organizing and problem-solving become more challenging.
- Stage 3: Mild to moderate cognitive decline is experienced, with worsening confusion and forgetfulness affecting daily tasks like dressing and cooking. Recall of names and events becomes difficult.
- Stage 4: Moderate Alzheimer’s stage marked by severe memory loss and the need for assistance with daily activities. Changes in personality and behavior, such as agitation, may occur.
- Stage 5: Moderate to severe cognitive decline requiring significant assistance with daily tasks. Patients may lose awareness of events or surroundings and may develop incontinence and significant changes in personality.
- Stage 6: Severe Alzheimer’s with profound cognitive decline, making communication extremely difficult. Patients may no longer recognize even close family members and require round-the-clock care and assistance with all activities of daily living.
What Happens After Stage 7 Alzheimer's?
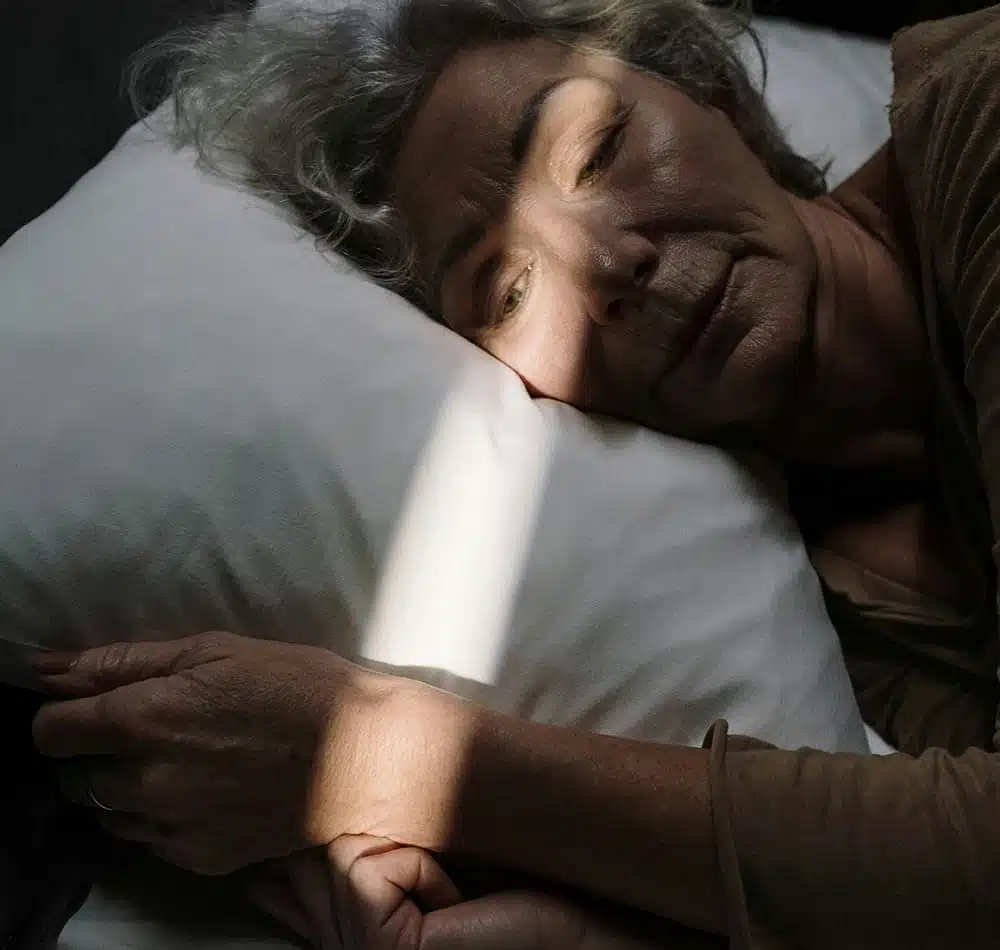
Once a patient reaches Stage 7 of Alzheimer’s, characterized by Severe Cognitive Decline, extensive care and support are needed as the end of life approaches. At this stage, the focus shifts towards providing comfort and maintaining dignity, as cognitive and communication functions are severely impaired. End-of-life planning and execution become essential, with a focus on symptom management and preserving the patient’s quality of life.
Physical complications that may arise in Stage 7 can significantly impact its timeline. Common complications include aspiration, pressure ulcers, pneumonia infections, and malnutrition, further exacerbating the decline of the individual. These complications often signal the progression towards the end of life.
Palliative care becomes paramount in Stage 7, aiming to alleviate symptoms and provide comfort in the final stages. This may involve pain management, maintaining skin integrity, ensuring proper nutrition and hydration, and offering emotional support to both patients and their loved ones as they navigate this challenging phase.
Ultimately, the management plan after Stage 7 of Alzheimer’s focuses on providing compassionate end-of-life care to ensure the patient’s last days are surrounded by love and support, allowing them to maintain their dignity.

Alzheimer’s Disease Timeline
Among Alzheimer’s patients, the progression of the disease varies, but there exists a general timeline for each stage. This timeline is characterized by a progressive decline in cognitive abilities, starting from mild symptoms in the early stages to more severe symptoms in the later stages. Late-stage Alzheimer’s is marked by severe cognitive deterioration, rendering patients completely dependent and unable to communicate effectively.
Efforts to slow the progression of Alzheimer’s and improve quality of life are crucial at all stages. This may involve engaging in appropriate levels of physical exercise, cognitive stimulation through games and activities, lifestyle changes such as improved diet and nutrition, and participation in engaging social activities to keep the mind active and the body strong. Additionally, medications such as cholinesterase inhibitors, when prescribed appropriately, can help manage symptoms and slow disease progression.
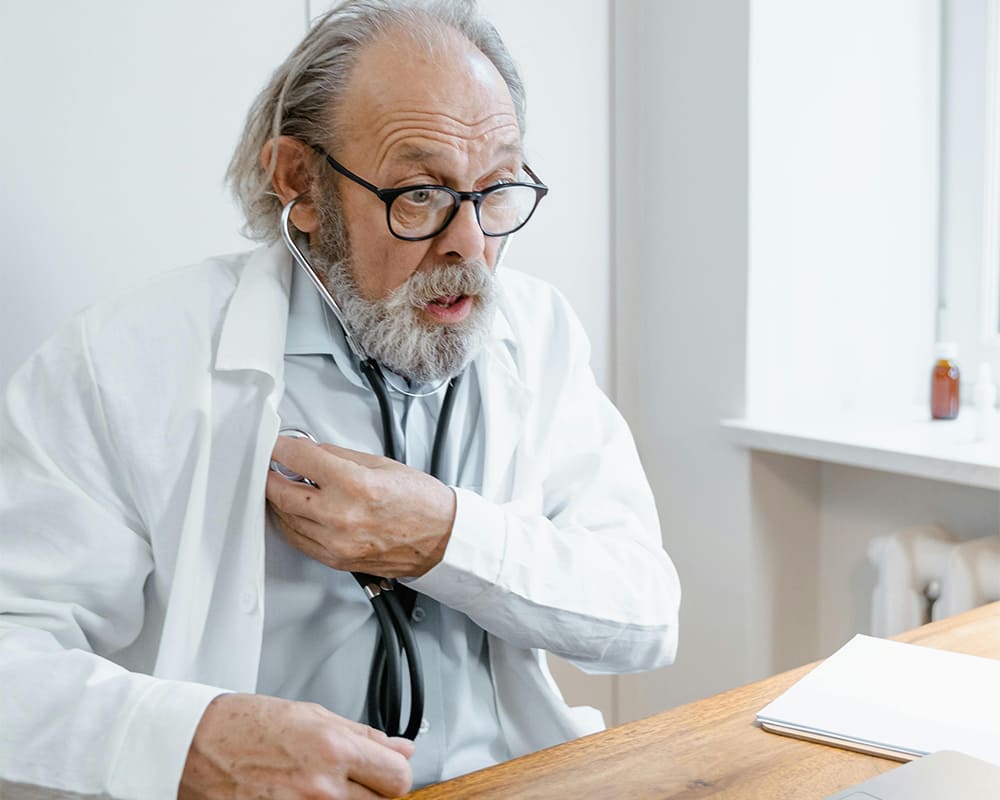
Each stage of Alzheimer’s requires comprehensive support from caregivers, healthcare professionals, and community resources. This support should encompass both practical assistance and emotional support for individuals with Alzheimer’s and those involved in their care. By implementing these strategies, caregivers can help slow the progression of Alzheimer’s in their patients while improving their overall quality of life.
Which Stage Of Alzheimer's Is The Longest?
The progression of Alzheimer’s between individuals differs vastly, making it difficult to pinpoint the longest stage. Statistically, though, Stage 1 and Stage 2, the early stages of Alzheimer’s involving mild cognitive decline, show the longest durations. The experience of subtle memory loss and mild concentration difficulties lasts for many years before advancing further. It’s imperative to understand that the length of time of each stage greatly factors in age, overall health, and genetic makeup. Carers need to pay attention to symptoms, request timely medical advice to better understand their patient’s experience, and adjust their management plan in light of the disease progression and effective supportive measures.
How Long Does Stage 7 Alzheimer's Last?
As with other stages, the duration of Stage 7, when severe cognitive decline in Alzheimer’s patients occurs, can vary from typically several months to several years. This is the stage of profound cognitive decline, with patients experiencing minimal to no ability to communicate for themselves or attend to basic tasks without assistance. Symptoms commonly experienced involve the loss of speech, facial recognition of loved ones, swallowing function, and incontinence.
Stage 7 focuses care strategies on making life as comfortable and dignified as possible for the dementia patient. Efforts to create calm and more familiar surroundings are implored, falls and injury prevention safety measures are taken, and proper hygiene management with diet and nutritional considerations prevail. Monitoring the effectiveness of these efforts with regular visits with healthcare professionals and hospice care teams is important for reassurance that appropriate measures are being taken and can bring attention to needed changes or new helpful information. This also ensures that respite care and emotional support are available and accessible to caregivers to ensure their own well-being in handling the challenges of this stage.
We Believe Prioritizing Brain Health Enhances Your Quality Of Life
Get to know our team, our mission and how our EVY LIGHT® can provide you and your loved ones with a fuller life, letting you breathe a little easier.
How Long Is Stage 6 Alzheimer's?
Like Stage 7, Stage 6 of Alzheimer’s can vastly differ between individual patients, again lasting from several months to a few years. This stage, commonly known as the stage of moderate to severe cognitive decline, is when profound cognitive loss is evident with much higher dependency on others to perform daily tasks. In Stage 6, patients suffer great memory loss, facial recognition difficulties of familiar people, and the loss of basic communication abilities.
Stage 6 Alzheimer’s care strategies call for comprehensive supervision in providing the support for various evolving individual needs. This involves an environment of increased structure and safety measures to ensure proper hydration and nutrition, medication management that also addresses anxiety and agitation, as well as ensuring the caregivers are sufficiently able to provide safe and proper assistance in daily living activities that involve bathing, dressing, and grooming. Aid from healthcare professionals is further required to suggest changes and adjustments to the care plans to address issues that arise while maintaining the best levels of quality of life and comfort that can be provided despite challenges.
Progression From Stage 6 To Stage 7
The progression to Stage 7 from Stage 6 is seen in significant digression of functional cognitive aptitude. The timeline of this progression differs between Alzheimer’s patients but is primarily evident in the degree of gradual deterioration over time. Pointers to this transition into Stage 7 include a further inability to communicate, requiring carers to fully assist in all activities of daily life, and the almost complete or total loss of recognition of loved ones and surroundings.
More extensive caregiving measures are required to support late-stage Alzheimer’s, with compassionate care and comfort maximization being at the forefront. Implementations may involve more stringent fall and injury safety measures, management of even higher degrees of aggression and agitation, and the proper administering of nutrition and hydration. Medical intervention may become more invasive while keeping the comfort of the patient paramount to manage increased pain. Palliative care efforts, coupled with regular healthcare professional monitoring, are imperative to immediately address issues that may arise from complications.
Overall, in transitioning from Stage 6 to Stage 7, more comprehensive care and support from all involved in the management of the Alzheimer’s patient is required in a concerted effort to provide the highest degree of comfort and dignity in living through the last stage of the Alzheimer’s disease.
Stage 5 Alzheimer's Memory
The stage of moderate cognitive decline issues in Stage 5 of Alzheimer’s. The individual experiences greater deterioration in memory that deeply affects daily life. Patients may feel tasked to recall vital personal information or recent happenings, forgetting their address or phone numbers. Short-term memory retention becomes apparent, causing the inability to take in new information or learn new tasks.
Adding to the memory loss of Stage 5 Alzheimer’s patients are the challenges they may face with executive functioning, for instance, planning, problem-solving, and decision-making. This may cause confusion and disorientation when introduced to new and unfamiliar surroundings. Frustrations caused by these short-term memory-related problems snatch their sense of safety and independence, requiring unwanted yet needed carer assistance with daily activities, resulting in further agitation and anxiety at the loss of individual identity to Alzheimer’s.
At Stage 5, the role of caregivers and healthcare professionals is vital in increasing the help and support to slow memory degradation. Alzheimer’s patients may need varied memory aids, consistency in their daily routine structure, and tools to handle the emotional toll on the individual experiencing memory loss challenges.
Transition Signs Between Seven Stages Of Alzheimer’s
The transition between the stages of Alzheimer’s can be recognized with keen understanding of changes observed in the individual’s functional and cognitive abilities. Some of these signs are increased memory loss, greater inability to complete daily tasks, and mood or behavioral changes. The speed of progression is impacted by factors such as age, overall health, and genetic predisposition.
The anticipation of greater needs in care management is essential in preparation to meet the challenges of Stage progression. Ensuring that access to appropriate medical and community resources is available to carers who need guidance and advice in proper modifications to living environments from healthcare professionals and support groups. Being proactive in taking on the challenges gives the caregiver a better chance at easing the transition between the stages of Alzheimer’s to provide optimal care both for themselves and the individual in their care.
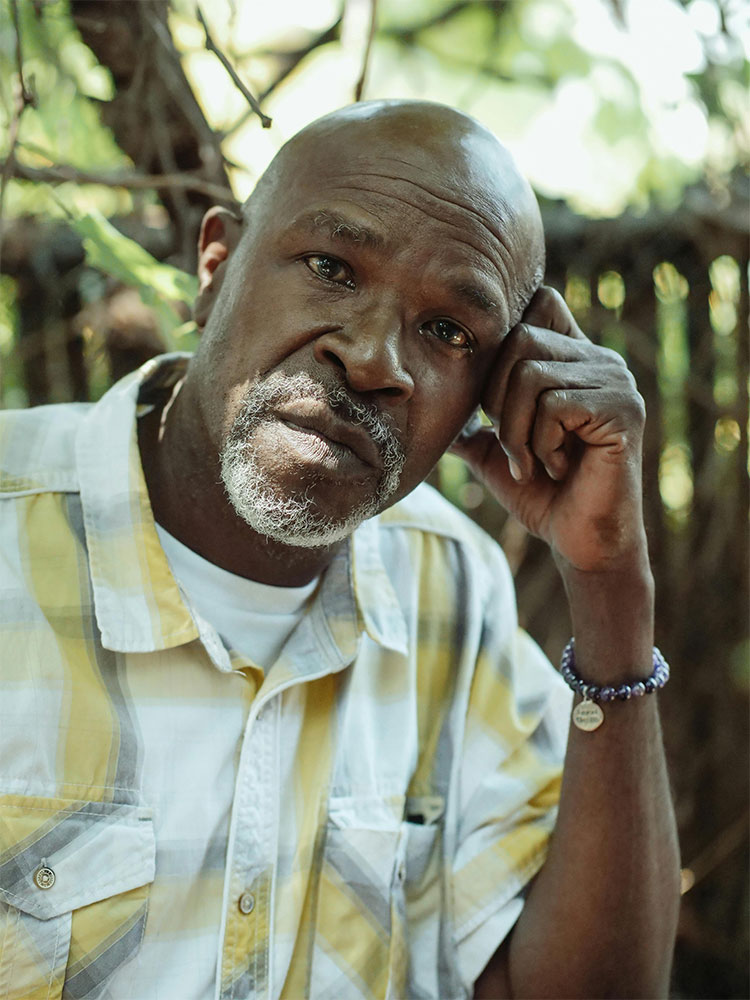
Impact of Alzheimer’s Progression On Patients And Families
The progression of Alzheimer’s brings on an unavoidable slew of emotional responses, ranging from feelings of frustration, anxiety, or depression as individuals grapple with the loss of memory and independence. Feeling helpless in witnessing these struggles has proven emotionally draining for loved ones who feel guilty and grief-stricken over it.
Systems to support families that provide emotional support and practical guidance through the stages are vital. These systems include counseling and support groups to share knowledge and experiences in coping. Open communication with healthcare professionals helps families feel more supported by providing better understanding and direction to navigate the intricacies of care decisions.
The care requirements for Alzheimer’s change as it moves towards the middle stages. New strategies may need to be adopted by families to address behavioral changes, communication challenges, and physical decline. This may involve measures that address issues of safety, memory care, hydration, and nutrition. In addressing the changing needs of both patients and families, care providers play an essential role in enhancing the quality of life for everyone involved as they navigate the rough terrain of Alzheimer’s Disease.

Enhance your brain performance through the power of light.
Comfortable and easy to use 40Hz light therapy to support and improve your brain function.
View Our LightAlzheimer's Life Expectancy
The question of life expectancy following an Alzheimer’s diagnosis depends significantly on many factors. Life after the Alzheimer’s diagnosis, on average, may span from 8 to 10 years, while various elements may either extend or shorten this lifespan in other patients.
The individual survival rate can be greatly affected by the overall health of the patient. As the disease advances, physical vulnerabilities increase the possibility of infections, falling, and malnutrition, which can cause steep declines in health with higher risks of fatality. Also, it is crucial at times to understand which sense is most affected by alzheimer’s disease.
Among the many factors that influence the progression of Alzheimer’s are lifestyle choices, genetics, and access to medical care. To slow this progression, measures that have been effective involve brain health promotion activities in the form of exercise, games, and social interaction. Thus, it is important to have brain exercises to prevent alzheimer’s. Additionally, susceptibility to Alzheimer’s and its outcomes is influenced by genetic factors, which are further impacted by access to quality medical care and appropriate treatments.
The comprehension of these factors aids the patient and families in making informed decisions on the best way forward in care and treatment options that support their ability to manage the challenges posed by Alzheimer’s.
Learn What Others Have Experienced with EVY Light
See how others have achieved a sharper mind by activating their gamma brainwaves in combination with maintaining a healthy lifestyle.
Frequently Asked Questions About How Long Do The 7 Stages Of Alzheimer's Last
How Long Do The 7 Stages Of Alzheimer's Last?
The progression of Alzheimer’s typically spans several years, with each stage marked by new symptoms and challenges indicating advancement to the next stage.
Which Stage Of Alzheimer's Is The Longest?
Statistically, though, Stage 1 and Stage 2, the early stages of Alzheimer’s involving mild cognitive decline, show the longest durations.