In this article, we will explore Alzheimer’s hallucinations, their triggers, and what would be a good management strategy to use to impact the quality of life. We will also learn to identify Alzheimer’s symptoms and learn about treatment tips.

Christopher Ravn
Key Takeaways
1. Hallucinations in Alzheimer's are sensory experiences that may worsen as the disease progresses, varying in frequency and type between early and late stages.
2. Triggers for Alzheimer's hallucinations include environmental changes, stress, medications, and underlying health conditions.
3. Managing Alzheimer's hallucinations involves creating a calm environment, medication (if needed), and therapeutic interventions.
Table of Contents
1. What Are Alzheimer’s Hallucinations?
2. Do Alzheimer's Patients Always Experience Hallucinations?
3. How Alzheimer’s Hallucinations Differ In Early Vs Late Stages
4. What Triggers Hallucinations In Alzheimer's?
5. Assessing The Risk Of Hallucinations In Alzheimer's Patients
6. Role Of Sleep Disorders In Alzheimer's Hallucinations
7. Can Alzheimer's Hallucinations Be Prevented?
8. 7 Tips To Managing Hallucinations In Alzheimer's
9. How Can Caregivers Effectively Respond To Hallucinations In Alzheimer Patients?
10. Are Medications Effective In Treating Alzheimer's Hallucinations? Treatment Options
11. Can Lifestyle Changes Reduce The Frequency Of Hallucinations In Alzheimer Patients?
12. What Is The Difference Between Alzheimer’s Hallucinations And Delusions?
13. Why Is It Important To Differentiate Between These Symptoms?
14. The Impact Of Hallucinations On Alzheimer’s Disease Outcomes
15. Frequently Asked Questions About Alzheimer's Hallucinations
What Are Alzheimer’s Hallucinations?
One of the most common types of dementia is Alzheimer’s disease. It leads to a decline in cognitive function, including memory and thinking, as well as changes in behavior. It can also cause hallucinations, which affect the patient and caregiver. Let’s explore the different types of hallucinations, their triggers, management strategies, and their impact on quality of life.
Hallucinations are a common symptom of dementia. It is a false perception that is experienced only by the individual and involves any of the senses from touch, sight, sound, taste, or smell, and that cannot be verified by anyone else
Although many might think that hallucinations and delusions are practically the same thing, it actually have varying definitions. Hallucinations are sensory experiences like seeing, hearing, or feeling things that aren’t really there. Delusions, on the other hand, are strong beliefs held firmly despite evidence to the contrary.
While one of the symptoms of Alzheimer’s disease can be delusions, hallucinations are more common.
- Visual hallucinations (seeing things that aren’t there) One of the common experiences is seeing things that aren’t there or real like people, animals, or objects
- Auditory hallucinations (hearing things that aren’t there) Hearing sounds or voices like music or conversations that aren’t there.
- Olfactory hallucinations (smelling things that aren’t there) Smelling things that aren’t real can be different from person to person and may be foul or pleasant
- Tactile hallucinations (feeling things that aren’t there) Feeling sensations that aren’t real on the skin
- Gustatory hallucinations (tasting things that aren’t there) Tasting things that aren’t there and including a metallic taste
Do Alzheimer's Patients Always Experience Hallucinations?
Alzheimer’s patients do not always experience hallucinations, though they may be present. It is not always a symptom of the condition. However, hallucinations are more prevalent in those with lewy body dementia (LBD).
At What Stage Do Hallucinations In Alzheimer’s Typically Occur? (H2)
While the hallucination can happen at any given time, research suggests that it usually happens at a later stage of the disease and becomes more frequent as it advances.
- Early Stage (Mild)
In the early stages of Alzheimer’s disease, hallucinations are not as common, occurring in less than 10% of individuals, where symptoms are often mild and may not be noticeable. - Middle Stage (Moderate)
As the disease worsens, hallucinations become more prevalent, affecting 20–30% of people either suddenly or over time. Stress, exhaustion, or sensory overload can cause hallucinations. - Late Stage (Severe)
Hallucinations are more frequent and severe in the advanced stages of Alzheimer’s disease, affecting up to 50% of individuals, and may affect multiple senses which can be distressing and frightening (seeing threatening figures, hearing disturbing voices).
The frequency and type of hallucinations differ between early and late stages of the disease.
How Alzheimer’s Hallucinations Differ In Early Vs Late Stages
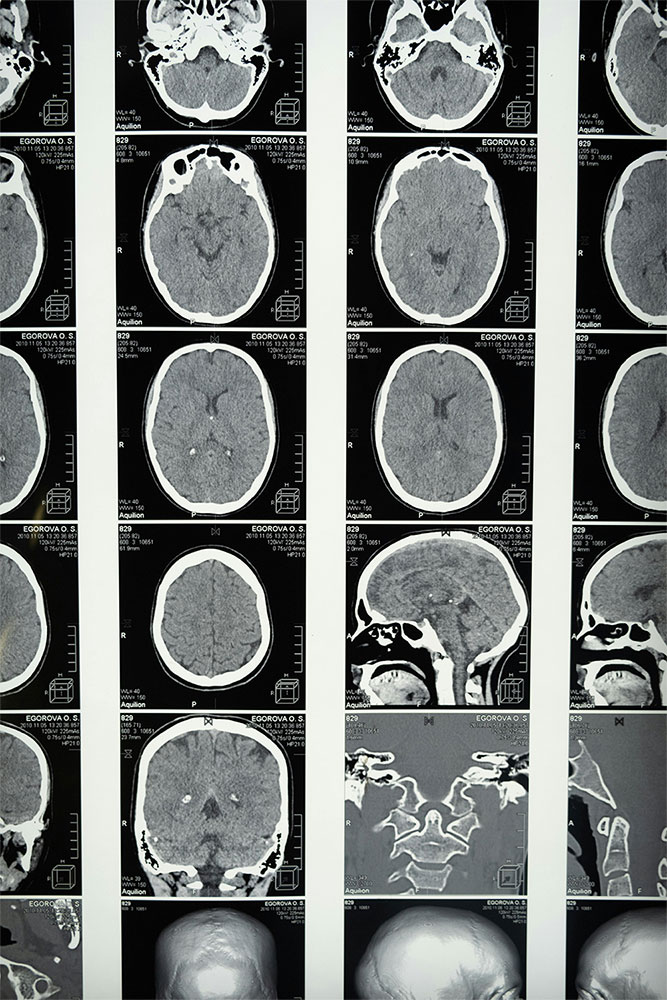
Hallucinations in Alzheimer’s disease are often linked to brain changes, including brain cell damage, neurotransmitter imbalance, sensory overload, and underlying medical conditions. While there is no cure for hallucinations, strategies to manage them include creating a calm environment, using antipsychotic medications, and using non-pharmacological interventions like reality orientation, music therapy for dementia, and validation therapy.
Causes of hallucinations include damage to the brain’s visual processing areas, reduced cholinergic input, and complex brain changes. Coping with hallucinations involves discussing illnesses and medications with the doctor, avoiding arguments, letting the person know they are safe, using a gentle touch, and explaining the person’s condition.
Alzheimer’s hallucinations are common, affecting 20-40% of patients. They differ between early and late stages, with early-stage hallucinations being less common and often triggered by sensory overload, confusion, medication side effects, and sleep disturbances. Late-stage hallucinations are often a sign of advanced cognitive decline and may be related to neurodegeneration, brain damage, medication side effects, and underlying medical conditions.
Some of the common triggers and experiences in early-stage patients and understanding these triggers can help to create a more suitable environment that is calmer and more predictable for early-stage Alzheimer’s which can help in reducing the level of intensity of the hallucinations.
- Stress, fatigue, and sensory overload
When the brain is overwhelmed, tired, or overly stimulated, their cognitive abilities are weakened which can lead to misinterpretations and trigger hallucinations. - Medication changes
The change and adapting to a new medication can disrupt brain chemistry, potentially triggering hallucinations. Always monitor the changes in behavior, if any and report accordingly to the healthcare practitioner. - Unrecognized pain
As the brain tries to make sense of the body’s signal when there is pain or discomfort, it sometimes might be translated as hallucinations when instead of pain in the hands, they might be “seeing” worms crawling on it.
What Triggers Hallucinations In Alzheimer's?
Hallucinations can be triggered by various factors, including changes in the environment, emotional stress, routine changes, sensory overload, sleep deprivation, social isolation, medications, health issues, sleep disorders, nutritional deficiencies, and other health conditions like Lewy body dementia, Parkinson’s disease, and other types of dementia. These changes can worsen hallucinations and may also result from medication side effects such as anticholinergic, antipsychotic, and sedative medications, health issues such as urinary tract disease, pain or discomfort, vision impairment, sleep apnea, nutritional deficiencies like vitamin B12, or other health conditions.
Assessing The Risk Of Hallucinations In Alzheimer's Patients
Hallucinations are a common symptom of Alzheimer’s disease, affecting 20-40% of patients. Identifying patients at higher risk is crucial for timely intervention and management. Genetic factors, such as APOE ε4 variations, and family history of Alzheimer’s disease or other dementias, may increase the risk of hallucinations. Environmental factors, such as sleep disturbances, sensory impairments, and medication side effects, can also increase the risk of hallucinations. Lifestyle factors, such as cognitive decline, social isolation, and high levels of stress and anxiety, can also contribute to hallucinations in Alzheimer’s patients. Identifying these factors is crucial for timely intervention and management.
Role Of Sleep Disorders In Alzheimer's Hallucinations
Sleep disturbances are a common symptom of Alzheimer’s disease, affecting both the patient and their caregivers. The prevalence of sleep disorders in Alzheimer’s patients is higher than in the general population and can appear early in the disease’s course. The most common sleep disorders include sleep breathing disorders, restless legs syndrome, periodic limb movements, insomnia, and REM sleep behavior disorder. Alzheimer’s patients frequently experience sleep apnea, restless legs syndrome, and periodic limb movements, while cognitive impairment, difficulty falling or staying asleep, and mood disturbances are symptoms of insomnia. Vivid dreams and sleepwalking are frequent symptoms of REM sleep behavior disorder, which is characterized by acting out dreams while asleep.
Can Alzheimer's Hallucinations Be Prevented?
There is no certain way to prevent dementia, but some ways to reduce the risk include maintaining a healthy lifestyle, managing chronic health conditions, getting enough sleep, and practicing stress-reducing techniques. While there is limited research on the prevention of hallucinations, some studies suggest that certain medications, such as cholinesterase inhibitors, may help reduce the risk. If your loved one is hallucinating, it is crucial to stay calm and maintain a safe environment. Reassurance, avoiding arguments, putting safety and comfort first, and taking medication if a doctor prescribes it are some tips. Ensure a clean, clutter-free environment with the correct temperature and brightness, encourage one-on-one time with others, and use a journal to record daily activities, moods, and behaviors and understand sensory activities for dementia patients. Consult with a healthcare professional if hallucinations become more severe or cause additional mood and behavioral shifts.
7 Tips To Managing Hallucinations In Alzheimer's
- Create a sleep-conducive environment in the bedroom, such as dark, quiet, and comfortable temperatures.
- Establish a consistent sleep schedule, ensuring the individual wakes up at the same time every day, including weekends.
- Encourage relaxation techniques, such as deep breathing, progressive muscle relaxation, or guided imagery, before bed. Limit naps to 30 minutes or less to avoid disrupting nighttime sleep.
- Avoid stimulating activities before bed, such as watching movies or engaging in intense conversations.
- Play soothing music in the background to create a relaxing atmosphere and promote better sleep.
- Monitor and adjust sleep patterns as needed, ensuring the individual reports any disturbances or discomfort to identify potential issues.
- Consult a healthcare professional for personalized advice on managing hallucinations and sleep disturbances in Alzheimer’s patients.
We Believe Prioritizing Brain Health Enhances Your Quality Of Life
Get to know our team, our mission and how our EVY LIGHT® can provide you and your loved ones with a fuller life, letting you breathe a little easier.
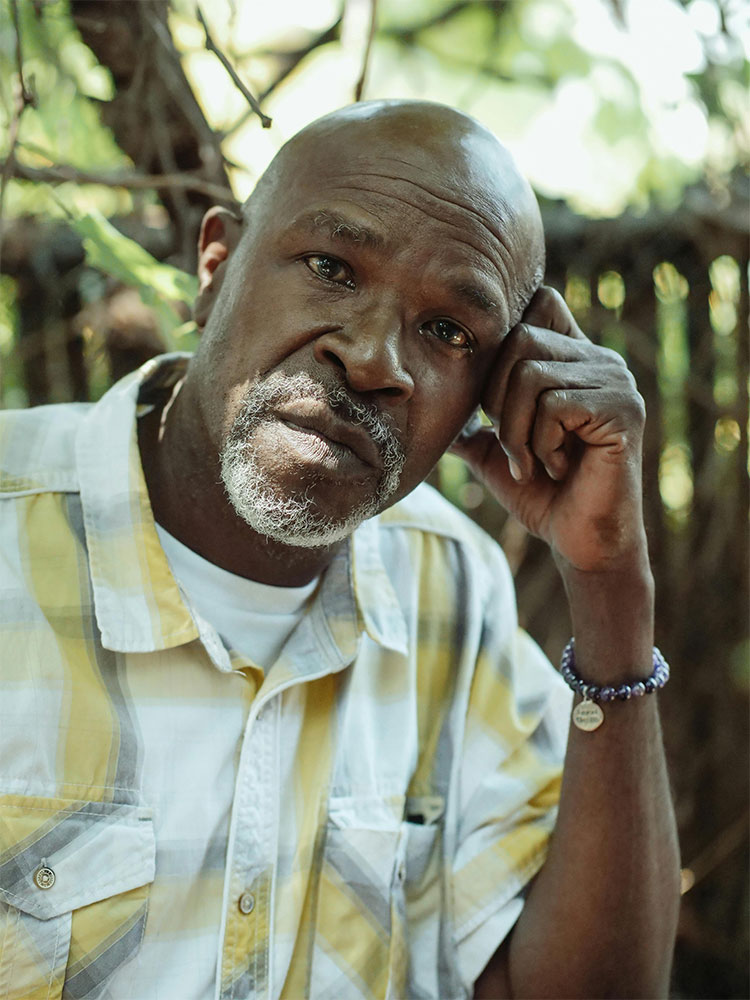
How Can Caregivers Effectively Respond To Hallucinations In Alzheimer Patients?
Caregivers should handle hallucinations calmly and safely to minimize distress and ensure the well-being of Alzheimer’s disease patients. To do this, caregivers should provide reassurance and understanding, investigate the immediate environment, use distraction, evaluate for medical causes, and create a safe and calm environment.
Practical tips include acknowledging the person’s feelings and concerns, investigating the environment to identify potential triggers, engaging the person in a different activity or conversation, consulting with the person’s healthcare provider, and creating a comfortable living space. Communication techniques include speaking calmly and clearly, using simple and clear language, avoiding arguing or dismissing the person’s hallucinations, focusing on the person’s feelings and concerns, and using non-verbal cues like a gentle touch or a calm presence to communicate empathy and reassurance.
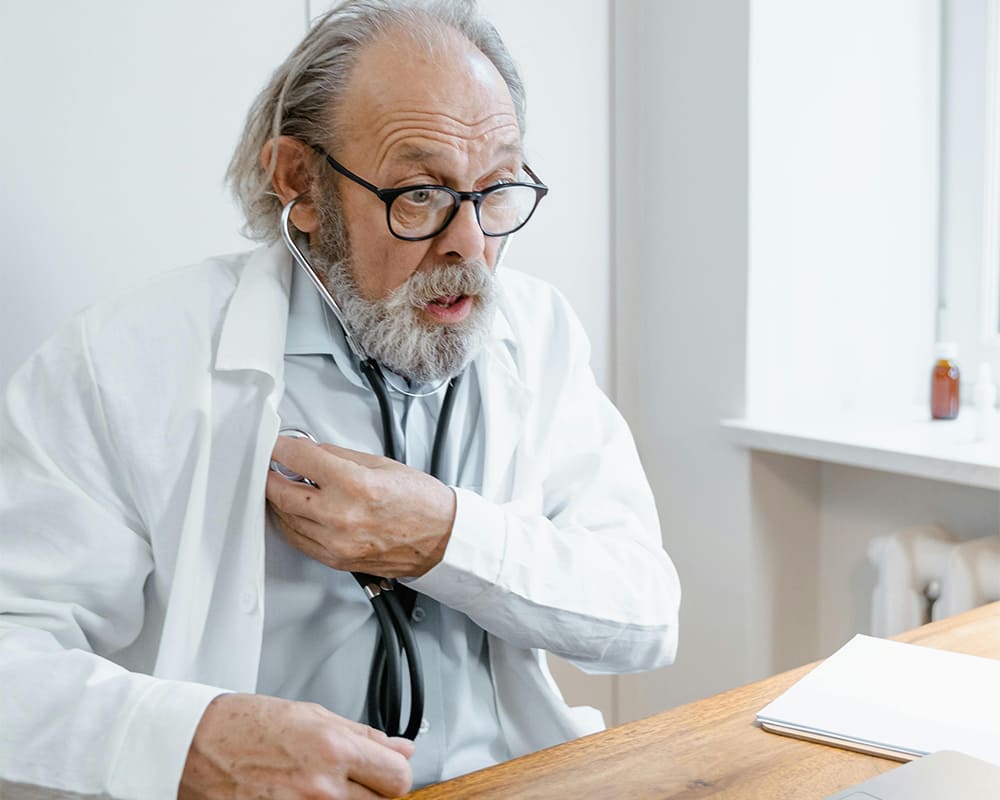
Are Medications Effective In Treating Alzheimer's Hallucinations? Treatment Options
Antipsychotics are commonly used to treat hallucinations in Alzheimer’s patients, but they come with serious side effects, including an increased risk of death in older adults with dementia-related psychosis. Rexulti, an antipsychotic medication, is approved for treating agitation associated with dementia due to Alzheimer’s disease, but it has common side effects like weight gain, sleepiness, dizziness, and restlessness. Other medications like cholinesterase inhibitors and memantine may also be used to manage symptoms but do not cure the underlying disease.
Pharmaceutic treatments offer relief from symptoms, improved quality of life, and the potential to slow disease progression. However, they also have risks, including increased risk of death in older adults with dementia-related psychosis, weight gain, sleepiness, dizziness, and potential for medication interactions and adverse reactions.
Can Lifestyle Changes Reduce The Frequency Of Hallucinations In Alzheimer Patients?
There is no diet that can completely reduce the frequency of hallucinations in Alzheimer’s patients, but a well-balanced diet rich in nutrients, including omega-3 fatty acids, antioxidants, and B vitamins, may help alleviate symptoms. These fatty acids have anti-inflammatory properties, which can reduce inflammation in the brain, which can contribute to hallucinations. Antioxidants, like vitamins C and E, protect against oxidative stress and damage to brain cells. B vitamins, particularly B12, are crucial for brain function and may reduce dementia symptoms. To add on, there are also brain exercises to prevent alzheimer’s.
To reduce stress and hallucinations in Alzheimer’s patients, it is essential to create a stable and comfortable environment. Maintaining a regular daily schedule, streamlining the environment, using calming colors and lighting, reducing noise and distractions, encouraging physical activity, offering emotional support, and routinely monitoring and addressing any underlying medical issues that may be causing hallucinations are all ways to achieve this. It is also beneficial to use light therapy for dementia.

Enhance your brain performance through the power of light.
Comfortable and easy to use 40Hz light therapy to support and improve your brain function.
View Our LightWhat Is The Difference Between Alzheimer’s Hallucinations And Delusions?
Hallucinations and delusions are common symptoms of Alzheimer’s disease, a type of dementia. Hallucinations are sensory perceptions that occur without external stimuli and affect any of the five senses, such as visual, auditory, olfactory, gustatory, and tactile. They can be vivid and realistic, making it difficult for the person experiencing them to distinguish between reality and fantasy.
Delusions are false beliefs that one clings to despite reality contradicting them. They can be related to paranoia and delusions, which can lead to anxiety, agitation, and aggression. Understanding the differences between hallucinations and delusions is crucial for effective management. Treatment approaches may vary depending on the underlying cause of the symptoms. For hallucinations, antipsychotic medications or other therapies can be used to reduce their frequency and intensity, while delusions may be addressed through cognitive-behavioral therapy (CBT) or other forms of psychotherapy to challenge and modify false beliefs.
Why Is It Important To Differentiate Between These Symptoms?
Differentiating between symptoms is crucial in diagnosing and managing complex conditions like depression, diffuse midline glioma, and rare CNS tumors. Accurate diagnosis allows healthcare providers to develop personalized treatment plans, significantly impacting patient outcomes. Symptoms can affect care approaches and treatment plans in several ways. For depression, accurate diagnosis using tools like the Beck Depression Inventory (BDI) or the Patient Health Questionnaire-9 (PHQ-9) allows for targeted treatment plans, including medication or psychotherapy, and monitoring patient progress.

The Impact Of Hallucinations On Alzheimer’s Disease Outcomes
Hallucinations in Alzheimer’s disease can have significant implications for both patients and caregivers. Studies have shown that hallucinations are associated with adverse consequences for patients, leading to a reduced quality of life and worse outcomes. These hallucinations, which are often visual, can result from brain damage and are more common in individuals with dementia with Lewy bodies or Parkinson’s disease dementia.
Furthermore, hallucinations and delusions can compromise the quality of life not only for patients but also for their caregivers. Delusions have been linked to greater caregiver burden, indicating that managing these symptoms can impact both the affected individual and those providing care.
Learn What Others Have Experienced with EVY Light
See how others have achieved a sharper mind by activating their gamma brainwaves in combination with maintaining a healthy lifestyle.
Frequently Asked Questions About Alzheimer's Hallucinations
What Are Alzheimer's Hallucinations?
One of the most common types of dementia is Alzheimer’s disease. It leads to a decline in cognitive function, including memory and thinking, as well as changes in behavior. It can also cause hallucinations, which affect the patient and caregiver. Let’s explore the different types of hallucinations, their triggers, management strategies, and their impact on quality of life.
Hallucinations are a common symptom of dementia. It is a false perception that is experienced only by the individual and involves any of the senses from touch, sight, sound, taste, or smell, and that cannot be verified by anyone else
Must Alzheimer's Patients Experience Hallucinations?
Alzheimer’s patients do not always experience hallucinations, though they may be present. It is not always a symptom of the condition. However, hallucinations are more prevalent in those with lewy body dementia (LBD).