Deciding when to transition a loved one with dementia or Alzheimer’s into a care home is a difficult choice filled with emotional complexities. While there’s no one-size-fits-all answer, recognizing key indicators can guide this decision. This guide explores those indicators, helping families weigh safety concerns, caregiving challenges, disease progression, and the individual’s needs to determine when a care home might be the most appropriate and supportive option.

Christopher Ravn
Key Takeaways
1. Recognizing signs like declining cognitive function, inability to perform daily tasks, and safety concerns can indicate the need for professional care in a memory care facility.
2. Caregiver burnout, characterized by emotional and physical exhaustion, is a significant challenge that may necessitate considering a care home.
3. Professional assessments, including mental status exams, help determine the severity of dementia and the appropriate level of care needed, guiding decisions about moving to a care home.
Table of Contents
1. When Should Someone With Dementia Go Into A Care Home?
2. When Should An Alzheimer's Patient Go To A Nursing Home?
3. What Are The Benefits Of Dementia Care Homes?
4. How Does Spending Time Affect The Quality Of Life For Dementia Patients?
5. What Financial Help Is Available For Dementia Sufferers?
6. When Should You Tell A Doctor About Memory Loss?
7. Frequently Asked Questions About When Should Someone With Dementia Go Into A Care Home
When Should Someone With Dementia Go Into A Care Home?
For a person with dementia, going into home care is a complex and emotional task. There is no standard answer, as it depends on factors such as the person’s needs, caregiver capacity, and the resources that are available. Thus, it is important to determine if the person is frequently getting lost, keeps on falling, has difficulty with basic self-care tasks such as dressing or eating, or is struggling to take their medication daily.
Recognizing The Signs
- Patients suffer from severe memory loss, confusion and disorientation
- Struggling with basic tasks such as eating, dressing, and using the washroom.
- Has increased behavioral issues such as aggression, wandering, hallucinations or paranoia.
- Feelings of overwhelm or being unable to cope with the demands of caregiving
- Safety and medical needs that require specialized care.
Family And Caregiver Challenges
- Seeing the gradual decline of a loved one is devastating.
- Physical demands in assisting with bats, dressing, mobility, and exercising can lead to exhaustion and sleep deprivation.
- Financial strain for caring for a loved one due to medical bills, home modifications, and assistive devices.
- Isolated from social circles as they dedicate more time to caregiving.
Professional Advice And Assessment
- Consult a healthcare professional, such as a geriatrician, neurologist, or psychiatrist, so that you know the stage and prognosis of the disease.
- Receive recommendations of care options such as home care, assisted living, or nursing home.
- Prescribe and monitor medications to manage symptoms.
- Provide emotional support and counseling to dementia patients and caregivers.
- Accesses a person’s cognitive function: memory, orientation, language, and attention span
- Determine severity of dementia and whether it is safe for them to care for themselves
When Should An Alzheimer's Patient Go To A Nursing Home?
- Safety concerns, such as the patient frequently wandering around and getting lost. This poses a safety risk and nursing homes provide secure environments around the clock.
- Alzheimer’s may impair balance and coordination, which makes the patient prone to falls and injuries. Therefore, considering a safer environment with trained staff is essential.
- The patient may struggle with self-care activities such as bathing, dressing, and eating. This places them at risk of poor nutrition.
- Caregiver burnout from physical and emotional exhaustion needs to be taken into consideration as well.
- The caregiver is unable to meet the needs due to physical limitations, a lack of resources, and time constraints.
- Severe cognitive decline in the patients is due to behavioral changes and mental needs.
Basic Tasks Of Daily Living
You will need to consider a nursing home when the basic tasks of daily living become difficult to complete. This would be eating, dressing, bathing, grooming, and using the washroom. Once there is a decline in the patient’s ability to perform their daily routine, there is an increase in their reliance on the caregiver, which impacts them emotionally and financially and increases their stress and exhaustion levels. It also raises concerns about the person’s well-being, dehydration, and infections. Thus, it is time for the Alzheimer’s patient to seek constant supervision and assistance from a nursing home.
Safety Concerns
- Wandering, which causes the patient to be lost. This is due to confusion, boredom, or a desire to return to a familiar place.
- Forgetting that they left the stove, oven, or even other appliances switched on.
- Unsafe driving places them at risk.
- Difficulty in understanding instructions and thus end up mixing their medication, which causes adverse health effects.
Medical Recommendations
- Cognitive decline such as inability to recognize faces, memory loss, issues with communicating, and impaired judgment.
- Issues with functional care such as bathing, dressing, eating, and using the washroom. They are also dependent on others for their daily living and have issues with managing their finances
- Behavioral changes such as agitation, aggression, and other challenging actions are difficult to manage at home. They also suffer from delusion, wandering easily, issues with sleep, and sundowning. It is also crucial to figure out what stage of dementia is sundowning in order to understand the dementia patients’ behavior better.
- They are also prone to falls and accidents, are unable to respond to dangerous situations, and have poor hygiene.
What Are The Benefits Of Dementia Care Homes?
The benefits of dementia care homes are that they provide specialized care and expertise with their trained staff and programs, and they provide round-the-clock safety and security. However, before enrolling the dementia patient into a care home, you will need to figure out how long can a person with dementia live at home. Dementia care homes also provide activities that are designed to keep the patient mentally, physically, and socially engaged. They can also participate in peer interaction with others, which helps to reduce feelings of loneliness and isolation. Moreover, placing a loved one in a dementia care home helps to reduce the stress and burden of caregiving and provides family members with peace of mind knowing that their loved one is well-cared for.
Professional Care And Supervision
- Round-the-clock supervision
- Staff can monitor and schedule the patients’ medication
- Health monitoring, such as reading vital signs or noticing changes in behavior.
- Specialized care if the patient has other medical conditions or training other than dementia.
Social Interaction And Activities
- It engages and challenges the brain, isolation, and depression, such as dabbling in puzzle games or discussions.
- Social interaction may help reduce feelings of loneliness, isolation, and depression, which are common in people with depression.
- Physical activities like gentle exercise, walking, or dancing boost mood, balance, and overall health.
- Encourage the patient to participate in social events to evoke a sense of purpose and belonging.
- Structure activities to help reduce signs of agitation, restlessness, and other challenging behavioral patterns.

Safety And Security
Care homes also provide safety and security, whereby they ensure that there are secure entrances and exits, technology that helps prevent wandering, staff available at all times, and access to an emergency call system or a panic button in the bathroom. The vicinity also has secured outdoor areas where residents are safe, code-locks, and color-coded hallways to help residents navigate themselves around.
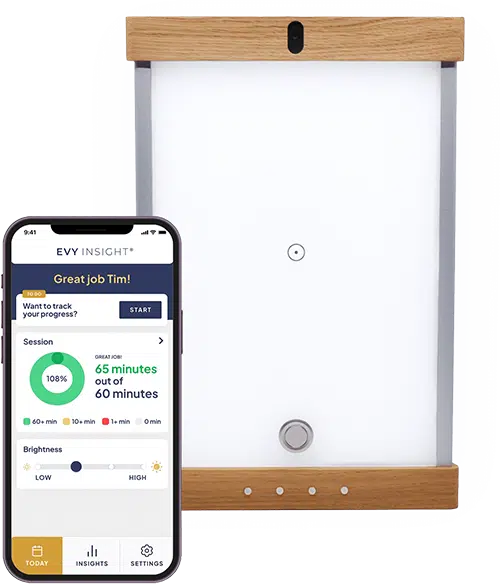
Join families who have found relief with EVY LIGHT®
Click below to see how EVY LIGHT® is helping others
How Does Spending Time Affect The Quality Of Life For Dementia Patients?
Spending time with dementia patients affects the quality of life, and dementia homes contribute to better living conditions because they prioritize safety and prevent falls, accidents, and wandering. It also provides personalized care, ensures that patients are always provided with balanced and nutritious meals, and assists with their personal care and hygiene.
Care homes also provide therapeutic activities and support to stimulate cognitive function, incorporate physical activities, organize social interactions to foster social connections, and provide emotional support to ensure that the residents feel heard and validated.
Life Expectancy Considerations
- Protocols are in place due to early detection and intervention, which helps extend life expectancy.
- Trained staff ensures accurate medication administration, reducing the risk of adverse effects.
- Fall prevention and other reduced risks of accidents are reduced, thus leading to fewer cognitive injuries or fatalities.
- Access to therapies and other physical, cognitive, and physical therapy helps to improve overall health.
What Financial Help Is Available For Dementia Sufferers?
- Medicaid which requires income and asset limits
- Medicare which applies to those who are 65 or older.
- Long-term care insurance, which covers dementia
- Veteran Affairs (VA) provides benefits for veterans with dementia
Planning For Long-Term Care
It is important to plan for long-term care as it helps to assist in covering dementia care, which is expensive, reduces financial stress, protects assets, and provides peace of mind for those who need to secure their future care. Hence, families need to plan and manage costs by seeking assistance from financial advisors, elder law attorneys, long-term care insurance, and government programs such as Medicare, Veterans Benefits, reverse mortgages, life insurance with long-term care riders, and annuities.
When Should You Tell A Doctor About Memory Loss?
It is important to tell a doctor about memory loss because it is important to determine the cause of it, determine if it is an early diagnosis of dementia, and plan and prepare individuals to plan for the future, including making any necessary arrangements.
The benefits of early diagnosis include allowing access to treatment, implementing lifestyle changes in diet and exercise, and accessing support services such as educational materials, support groups, and counseling. It is also to ensure regular monitoring to track the prevalence of the diseases and adjust care plans where needed.
It is time to consult a doctor about memory loss when you or your loved ones start showing signs of forgetfulness, struggling with routine activities such as paying the bills, changes in mood such as anxiety and depression, difficulty in communicating, feeling disoriented, making an impulsive decision and neglecting one’s hygiene.
Frequently Asked Questions About When Should Someone With Dementia Go Into A Care Home
When Is It Time To Go To A Nursing Home With A Dementia Patient?
- Safety concerns, such as the patient frequently wandering around and getting lost. This poses a safety risk and nursing homes provide secure environments around the clock.
- Dementia may impair balance and coordination, which makes the patient prone to falls and injuries. Therefore, considering a safer environment with trained staff is essential.
- The patient may struggle with self-care activities such as bathing, dressing, and eating. This places them at risk of poor nutrition.
- Caregiver burnout from physical and emotional exhaustion needs to be taken into consideration as well.
- The caregiver is unable to meet the needs due to physical limitations, a lack of resources, and time constraints.
How Does Spending Time Affect The Quality Of Life For Dementia Patients?
Spending time with dementia patients affects the quality of life, and dementia homes contribute to better living conditions because they prioritize safety and prevent falls, accidents, and wandering. It also provides personalized care, ensures that patients are always provided with balanced and nutritious meals, and assists with their personal care and hygiene.