Lewy body dementia (LBD) and Parkinson’s disease (PD) are two distinct neurodegenerative disorders with overlapping symptoms, making diagnosis challenging. This comprehensive guide will delve into the key differences between LBD and PD, exploring their unique symptoms, diagnostic challenges, misdiagnosis rates, progression, and risk factors. Understanding these distinctions is crucial for accurate diagnosis and appropriate treatment of these debilitating conditions.

Christopher Ravn
Key Takeaways
1. Lewy body dementia (LBD) and Parkinson's disease (PD) are distinct neurodegenerative disorders with overlapping symptoms, leading to frequent misdiagnosis.
2. LBD primarily affects cognition, while PD primarily affects motor function, but both can lead to cognitive decline, sleep disturbances, and emotional distress.
3. Early diagnosis and tailored treatment plans are crucial for managing both LBD and PD and improving the quality of life for patients and caregivers.
Table of Contents
1. How Does Lewy Body Dementia And Parkinson’s Disease Differ?
2. What Are The Diagnostic And Misdiagnosis Challenges Between Lewy Body Dementia Vs. Parkinson’s?
3. How Often Is Lewy Body Dementia Misdiagnosed As Parkinson's?
4. How Can You Tell The Difference Between Parkinson's Disease Vs. Lewy Body Dementia?
5. Can Parkinson's Turn Into Lewy Body Dementia?
6. What Percentage Of Parkinson's Patients Get Lewy Body Dementia?
7. How Does Lewy Body Dementia (LBD) Affect Sleep Compared To Parkinson’s?
8. Lewy Body Dementia Vs. Parkinson’s Impact On Quality Of Life
9. What Are The Early Signs And Symptoms Of Lewy Body Dementia Vs Parkinson’s?
10. Who Is At High Risk For Lewy Body Dementia?
11. What Is The Prognosis And End-Stage Like For Lewy Body Dementia Vs. Parkinson’s Disease?
12. Is Lewy Body The Worst Dementia?
13. Frequently Asked Questions About Lewy Body Dementia Vs Parkinson
How Does Lewy Body Dementia And Parkinson’s Disease Differ?
Lewy body dementia (LBD) is when there is an abnormal protein called Lewy bodies found in the brain. This protein works by disrupting the function of the brain, which causes one to experience issues with cognition, motor skills, and behavior. Parkinson’s disease (PD), on the other hand, is a neurodegenerative disorder that affects a person’s movement, balance, and coordination. This is because the neurons that produce dopamine in the brain start to deteriorate.
- Cognitive issues such as memory loss, conduction, and mood changes
- Motor issues such as having tremors, being unable to balance, and feeling rigid.
- Behavioral issues like hallucinations and sleep problems.
- Motor issues such as feeling rigid, posture issues, and slow movement (bradykinesia)
- Non-motor issues such as depression, anxiety, sleep issues, and cognitive impairment.
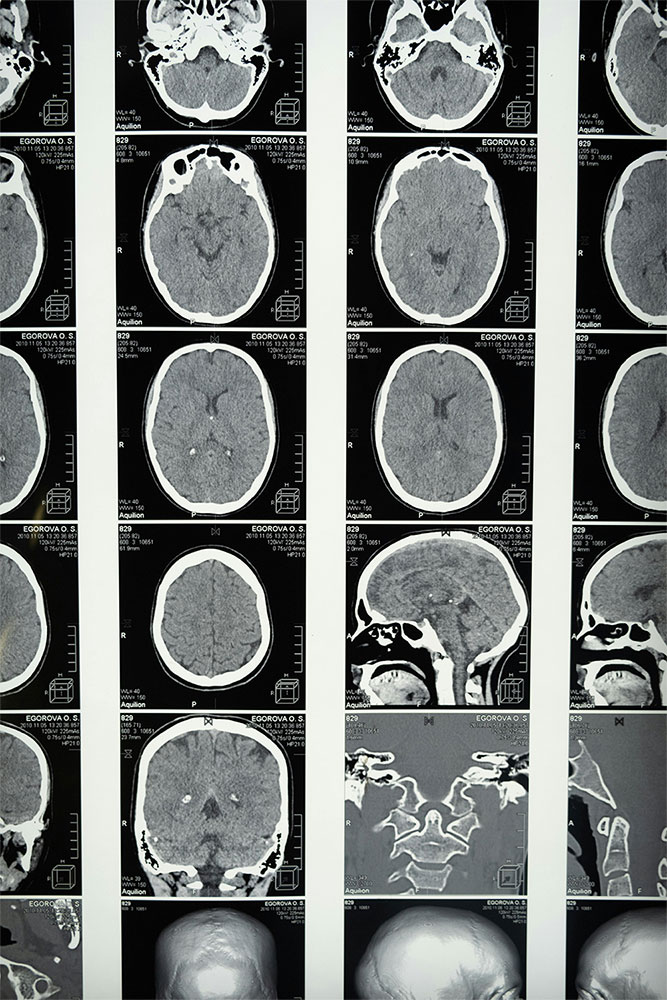
What Are The Diagnostic And Misdiagnosis Challenges Between Lewy Body Dementia Vs. Parkinson’s?
LBD and PD are two separate neurodegenerative disorders and they show similarities in their symptoms.
Fluctuating cognitive impairment: Both LBD and PD can exhibit fluctuating cognitive impairment, making it difficult to distinguish between the two conditions. PD can be misdiagnosed as LBD due to tremors, feelings of rigidity and bradykinesia, signs of dementia, and a lack of proper diagnostic tests.
On the other hand, LBD can be misdiagnosed as PD because it shows signs of Parkinsonism and the presence of cognitive impairment, and most times, it is a failure to recognize LBD.
How Often Is Lewy Body Dementia Misdiagnosed As Parkinson's?
The rate at which Lewy Body Dementia (LBD) is often misdiagnosed as Parkinson’s Disease (PD) can range from 20% to 50%. This is because both diseases share similar symptoms, such as cognitive impairment and insufficient diagnostic tests because they are based on clinical evaluation. Moreover, LBD tends to showcase itself as Alzheimer’s disease, which poses a challenge during diagnosis and shows up differently in different individuals. This makes it difficult to diagnose LBD in a proper manner.
Join families who have found relief with EVY LIGHT®
Click below to see how EVY LIGHT® is helping others
How Can You Tell The Difference Between Parkinson's Disease Vs. Lewy Body Dementia?
- Onset symptoms for PD: Tremors, rigidity, and bradykinesia.
- Onset symptoms for LBD: Memory loss, attention deficits, and hallucinations before motor issues.
- Cognitive decline in PD is slow and gradual and manifests itself as dysfunction, attention deficits, and memory loss.
- Cognitive decline for LBD is rapid and noticeable showcasing memory loss, attention deficits, and hallucinations
- LBD hallucinations occur in the context of visual, auditory, or tactile.
- PD has sleep problems like insomnia and restless leg syndrome.
- LBD has sleep issues, such as rapid eye movement (REM) sleep, and behavioral issues.
Can Parkinson's Turn Into Lewy Body Dementia?
Both PD and LBD have an abnormal protein in the body known as Lewy bodies. This is an abnormal protein that accumulates and aggregates in the brain. Lewy bodies are a feature of LBD and are seen in some cases of PD. The conditions that underlie both PD and LBD are still not understood, as they present their own set of complexities.
- It is common to view Lewy Bodies in the brain for both PD and LBD patients
- The risk of PD patients who have a family history of LBD will most likely develop LBD
- The accumulation of a protein called α-synuclein is the primary progressor of Lewy bodies.
What Percentage Of Parkinson's Patients Get Lewy Body Dementia?
It has been stated that approximately 80% of people with Parkinson’s Disease will get Lewy Body Dementia. The Journal of the American Medical Association (JAMA) said the prevalence of dementia with Lewy bodies (DLB) in those with Parkinson’s disease was 14.4 per 1000 people.
Lewy body dementia (LBD) is a common complication of Parkinson’s disease (PD), with estimates suggesting that up to 80% of people with PD will develop LBD at some point in their lives. However, the exact percentage of PD patients who develop LBD is difficult to determine due to the complexity of the disease and the varying definitions of LBD.
- Those who are of older age
- Men are more likely to develop LBD
- Those who have the APOE ε4 allele
- A family history of LDB or PD
- Patients who show levels of cognitive impairment
Comparative analysis with other forms of dementia includes Alzheimer’s Disease (AD) and frontotemporal dementia (FTD). Though LBD may show the same traits as other dementia, it has different features, such as
LBD is often compared to other forms of dementia, including Alzheimer’s disease (AD) and frontotemporal dementia (FTD). While LBD shares some similarities with these conditions, it has distinct clinical and pathological features, such as being more likely to be linked with visual hallucinations and fluctuations. However, AD would be more likely to be linked with loss of memory and language difficulties.
How Does Lewy Body Dementia (LBD) Affect Sleep Compared To Parkinson’s?
Both Parkinson’s disease and Lewy body dementia (LBD) disrupt sleep, but LBD is different because it causes vivid dreams, nightmares, and REM sleep behavior disorder (RBD), where people physically and occasionally violently act out their dreams. Excessive daytime sleepiness is also more common in LBD. Parkinson’s, however, is associated with insomnia, restless legs syndrome, sleep apnea, and nocturia. Both conditions require medical attention for diagnosis and treatment.
LBD significantly impacts sleep, primarily due to RBD. This disorder causes vivid dreams and a lack of muscle paralysis during REM sleep, leading to the physical enactment of dreams. RBD can manifest as talking, walking, or even violent outbursts, disrupting sleep.
Insomnia and fragmented sleep are also common in LBD, often due to cognitive impairment, depression, anxiety, and the disruptive nature of RBD, contributing to excessive daytime sleepiness.
Impact Of Parkinson’s On Sleep Patterns
Parkinson’s disease (PD) significantly affects sleep, causing issues like insomnia, daytime sleepiness, sleep fragmentation, REM sleep behavior disorder (RBD), sleep apnea, and restless leg syndrome (RLS). These disturbances stem from the disease itself, medications, nocturnal motor symptoms, co-existing conditions, and aging.
Medications used to treat PD can worsen sleep problems. Dopamine agonists and levodopa can cause sedation or insomnia, while anticholinergics and benzodiazepines might cause sedation and worsen sleep apnea. Stimulants, although helpful for daytime alertness, can disrupt sleep.
Treatment options for sleep disturbances in PD include cognitive behavioral therapy for insomnia (CBT-I), melatonin, stimulants, sleep aids, light therapy for cognitive decline, and lifestyle changes.
Lewy Body Dementia Vs. Parkinson’s Impact On Quality Of Life
Lewy body dementia (LBD) and Parkinson’s disease (PD) are neurodegenerative disorders that significantly impact quality of life. Both conditions can cause cognitive impairment, motor symptoms, and sleep disturbances. However, LBD often presents with cognitive decline first, while PD typically begins with motor symptoms. At this stage, it is important to understand how to help someone with cognitive impairment. LBD is also characterized by fluctuations in alertness and cognition, and visual hallucinations are more common than in PD.
LBD and PD both lead to cognitive decline, affecting daily activities and relationships. Motor symptoms can hinder everyday tasks, and sleep disturbances negatively impact mood and energy levels. Both conditions can cause emotional distress and burden caregivers.
Early diagnosis, medication, non-pharmacological interventions, caregiver support, and lifestyle modifications are crucial for managing these conditions and improving quality of life for both individuals and their caregivers.
Quality Of Life In LBD Patients
Lewy body dementia (LBD) severely impacts patients’ lives, causing cognitive, motor, and behavioral decline. Patients may experience memory loss, confusion, difficulty with movement, hallucinations, and mood swings, leading to a diminished quality of life and challenges in daily activities, relationships, and independence.
LBD also has a profound psychological and emotional impact on patients, causing anxiety, depression, loss of identity, fear, uncertainty, and grief. They may struggle with losing control, their changing sense of self, the progression of the disease, and the impact on loved ones.
Caregivers of LBD patients also face emotional burdens, including stress, guilt, anxiety, loss of identity, and emotional distress. The demands of caregiving can lead to exhaustion and feelings of inadequacy, further impacting their well-being.

Quality Of Life In Parkinson’s Patients
Parkinson’s disease (PD) significantly impacts quality of life (QOL), affecting motor function, cognition, sleep, and mental health. Tremors, rigidity, and balance issues can hinder daily activities. Cognitive impairment, depression, anxiety, and sleep disturbances further diminish QOL.
Lewy body dementia (LBD) patients share many QOL challenges with PD patients, including cognitive impairment, motor symptoms, sleep disturbances, and emotional distress. However, LBD patients often experience more pronounced cognitive decline, impacting daily life and social interactions more significantly. While PD patients generally have more severe motor symptoms, both conditions can affect mobility. LBD patients may also experience more severe sleep disturbances and are potentially more prone to depression and anxiety due to their greater cognitive decline.
What Are The Early Signs And Symptoms Of Lewy Body Dementia Vs Parkinson’s?
Though LBD and PD are different in terms of neurodegenerative disorders, they have some symptoms that are similar. Moreover, early symptoms of Lewy body dementia vs. Parkinson’s disease include rigidity, slow movement (bradykinesia), postural instability, memory issues, an inability to concentrate, verbal issues, issues with sleep such as insomnia, REM sleep behavior disorder, and restless leg syndrome. However, the early symptoms of LBD are cognitive issues, hallucinations, constant falling, and REM sleep behavior. In terms of PD, there are motor issues first, then cognitive decline and fluctuation, and a few falls.
What Are The First Signs Of A Lewy Body?
- Issues with remembering events or new details.
- Hallucinations
- Sudden changes in energy or alertness.
- Issues with movement. Patients may experience stiffness or rigidity.
- Issue with sleep or sleeping a lot during the day.
- Unable to balance, coordinate, or even have issues swallowing food.
- Sudden mood swings, confusion, or disorientation.
The differences in early presentation compared to Parkinson’s disease (PD) are at times, LBD may show signs of cognitive issues, such as higher rates of visual hallucinations and sleep issues. It also tends to be faster in its progression compared to PD.
A case study would be a 65-year-old woman who showed signs of depression and anxiety. However, during the course of time, the patient started experiencing recent events or even conversations that they had with their loved ones. There were also subtle signs that they were seeing people from the past.
What Are The First Signs Of Parkinson’s Disease?
- Sudden movements while they were asleep, such as twitching or jerking,.
- The movement slows down (bradykinesia), which can be seen while getting out of bed or walking.
- Unable to smile, blink, or even swing their arms.
- Issues with balance and coordination in older patients.
Differences in early presentation compared to Lewy Body Dementia (LBD) are that PD mainly focuses on motor issues such as tremors, rigidity, and bradykinesia. However, LBD showcases issues that are linked with behavioral symptoms and cognitive issues such as memory loss, hallucinations, confusion, problem-solving issues, and severe sleep problems such as insomnia or sleeping excessively throughout the day.
While Parkinson’s disease and Lewy Body Dementia (LBD) share some similar symptoms, there are key differences in their early presentation:
An example would be a 65-year-old retired engineer who experienced issues getting out of bed in the morning and walking. There were times when his hands trembled while he was eating breakfast. He was later diagnosed with Parkinson’s after a consultation with the doctor.
What Is The One Year Rule For Lewy Body Dementia?
The one-year rule for Lewy body dementia (LBD) is that it is used to distinguish between Dementia with Lewy Bodies (DLB) and Parkinson’s Disease Dementia (PDD). This rule states that if dementia symptoms come up during the first year of the onset of dementia, then they are classified as DLB. However, if Parkinson’s disease continues for more than one year after the onset of dementia, it is called PDD.
The relevance of the diagnosis is that it would help healthcare professionals completely determine if it is DLB or PDD. This is because each of these symptoms must have a different treatment and prognosis. Cholinesterase inhibitors are used to treat DLB, while dopamine replacement therapy is used to treat PDD.
The one-year rule is crucial in clinical diagnosis and is important for those who exhibit a rapid cognitive decline. This may be seen with the patient hallucinating or having fluctuations in attention. However, for PDD, this is often seen in slower cognitive decline with issues such as rigidity and bradykinesia.
There is, however, an exception to the rule, such as the fact that some DLB patients may exhibit a slower or faster decline in their cognition. This makes it an issue to tell PDD and DLB.
Who Is At High Risk For Lewy Body Dementia?
- Risk increases with age, especially after age 50.This can also be linked to early signs of Alzheimer’s in 50’s.
- Men are more susceptible to LBD than women.
- Those who have a family history of LBD or PD may have an increased risk of LBD.
- Genetic genes such as GBA or APOE
- Health issues such as high cholesterol, diabetes, or high blood pressure History of anxiety and depression
- There is little exercise and low dietary intake of omega-3 fatty acids and saturated fats.
- Brain injury or medications such as anticholinergics and benzodiazepines
Can You Have Lewy Body Dementia And Not Have Parkinson's?
- When did dementia and Parkinsonism enter a patient’s life? That is, whether dementia preceded Parkinsonism or did Parkinsonism precede dementia?
- Is Parkinsonism milder or more severe than PD?
- Fluctuations in cognitive and motor symptoms
- Hallucinations are often seen in LBD, compared to PD.
What Is The Prognosis And End-Stage Like For Lewy Body Dementia Vs. Parkinson’s Disease?
Though LBD and PD have some similarities, they have differences in their prognosis and end-stage symptoms.
After being diagnosed with LBD, the average survival time is around 5–7 years. However, there are those who may live up to 15 years.
Advanced stages of LBD may showcase issues such as memory loss, confusion, speech, depression, anxiety, dependence on caregivers for their daily routines, hallucinations, delusions and changes in behavior.
As for PD, the prognosis is that once diagnosed, a person can live around 10-15 years but there have been cases where some have lived to 20 – 30 years.
The end-stage for PD is that they experience severe issues such as tremors and rigidity, memory and attention issues, speech difficulty, fall risk, and need help from caregivers for their daily activities.
What Is The Dying Process With Lewy Body Dementia?
- The early stage exhibits hallucinations, sleep issues, and even acting out one’s dream
- The middle stage exhibits cognitive issues, severe confusion, and issues with their daily activities. It is also possible that patients show Parkinsonian symptoms such as balance, tremors, and even rigidity.
- The advanced stage exhibits severe cognitive issues, being unable to communicate, and dependence on caregivers. They may also showcase issues with eating, breathing, and even swallowing.
At the end of life, patients may exhibit an inability to respond to their environment, infections, and other complications. Thus, it is important to expect that patients will exhibit pain, issues with communicating, being unable to have autonomy, and emotional issues. Therefore, it is important that palliative care be considered to manage their pain, hallucinations, and delusions, provide emotional support, and help caregivers plan for end-of-life care and even hospice care.
Families and caregivers need to be educated to understand the disease and its progression, respite care for caregivers to recharge, counseling sessions to cope with emotional challenges, and hospice care to provide extensive care and support for the patients and their families during the end-of-life journey.
What Is The Dying Process With Parkinson’s Disease?
- The early stages are when a patient manifests symptoms such as tremors, bradykinesia, and instability with their posture.
- In the maintenance stage, medication is introduced to manage issues such as balance and coordination, speech and swallowing, bradykinesia, tremors, and rigidity.
- The advanced stage is when the symptoms worsen, such as immobility, tremors, rigidity, issues with communication, swallowing food, a higher risk of falls and injuries, and issues with activities such as dressing or combing their hair. They may also experience problems like depression and anxiety.
Is Lewy Body The Worst Dementia?
- LBD patients exhibit hallucinations, cognitive decline, and Parkinsonian symptoms. The symptoms are unique compared to other dementias.
- Alzheimer’s Disease exhibits a progression in memory loss, inability to communicate, and inability to solve problems.
- Vascular dementia occurs when there is reduced blood flow to the brain. This leads to memory loss and decreased cognition and communication.
- Frontotemporal dementia, on the other hand, is seen in changes in one’s behavior, personality, cognitive decline, and behavior.
The quality of life for LBS is lower than other forms of dementia. AD, on the other hand, has a longer survival rate and slower progress. Vascular dementia has a slow cognitive decline but more physical symptoms. As for frontotemporal dementia, it has a more progressive decline in cognitive function and daily life.
A study found that people with LBD had lower life quality compared to those with AD. It has a shorter survival time and is a burden on caregivers.
Frequently Asked Questions About Lewy Body Dementia Vs Parkinson
What Is There To Know Between Lewy Body Dementia Vs. Parkinson's Disease?
Lewy body dementia (LBD) is when there is an abnormal protein called Lewy bodies found in the brain. This protein works by disrupting the function of the brain, which causes one to experience issues with cognition, motor skills, and behavior. Parkinson’s disease (PD), on the other hand, is a neurodegenerative disorder that affects a person’s movement, balance, and coordination. This is because the neurons that produce dopamine in the brain start to deteriorate.
Is It Possible For Lewy Body Dementia To Be Misdiagnosed As Parkinson’s?
LBD can be misdiagnosed as PD because it shows signs of Parkinsonism and the presence of cognitive impairment and most times, it is a failure to recognize LBD.